'Aliah's GIT & HB Systems1
-
Upload
luqman-al-bashir-fauzi -
Category
Documents
-
view
242 -
download
0
Transcript of 'Aliah's GIT & HB Systems1
-
8/9/2019 'Aliah's GIT & HB Systems1
1/33
-
8/9/2019 'Aliah's GIT & HB Systems1
2/33
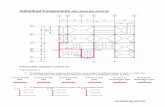
GENERAL HISTOLOGY OF GIT
PORTIONS DETAILS
ORGANS OFGIT
Oral cavity (ingestion & initial fragmentation) pharynx esophagus (deglutition & peristalsis) stomach (complete
fragmentation & initial digestion) small intestine (complete digestion & major absorption) large intestine (water
absorption) rectum (hold feces) anal canal (defecation).
LAYERS FACTS APPLIED ANATOMY
MUCOSA
y Sometimes known as mucous membrane.
y Further divided into 3 sublayers:1. Epithelial lining.2. Lamina propia:
Loose connective t/s.
Rich in blood vessels, nerves, & lymphatics. More collagenous in esophagus.
3. Muscularis mucosae:
Several layers of smooth m/s.
Functions:a. Keeps e mucosal surface & gland in constant state of gentle
agitation.
b. Prevents clogging.c. Enhances contact b/w epithelium & luminal content for absorption.
y 4 basic mucosal types according to main functions:1. Protective:
Stratified squamous epithelium non-keratinized. Mainly at upper GIT (oral cavity, pharynx, & esophagus) & anal canal,
where e lining is continuous with e skin.
2. Secretory: Lined by long, closely packed tubular gland.
Only at stomach.
3. Absorptive:
Lined by villi to increase surface area of absorption. Absorptive cells r tall columnar with striated (brush) border. Seen in small intestine.
4. Absorptive & protective: Closely packed straight tubular glands consisting of goblet cells which
lubricate e passage of feces.
Seen in e whole large intestine.
y 4 points along GIT where e mucosa undergoes abrupt transition from oneanother:1. Esophago-gastric junction.
2. Gastro-duodenal junction.3. Ileo-cecal junction.4. Recto-anal junction.
y Abundant lymphoid nodules or
aggregation in lamina propia &submucosa layer against bacterialinvasion.
y Exception for e oral cavity,esophagus, & anal canal.
y E entire digestive tract is lined by
a simple thin & vulnerableepithelium.
y
Zone just below e epithelium isrich in macrophages & lymphoidcells.
y These lymphoid cells produceantibody which is secreted into e
lumen to against viral & bacterialinvasion.
SUBMUCOSA
y Loose connective t/s supporting e mucosa.
y Contents:1. Blood vessels, lymphatics, & nerves.
2. Meissners plexus: contains postganglionic sympathetic fibers arising from esuperior mesenteric plexus.
3. Parasympathetic ganglion cells with postganglionic fibers which supply e
mucosal glands & e smooth m/s of e muscularis mucosae.
y A rich network of pre &
postganglionic fibers of ANS &some visceral sensory fibers inthese ganglia permit
communication b/w them.
y E no. of ganglion is numerous in
region where motility i s e greatest.
y Dx like Hirschsprung;s Dx or
Chagas Dx, e digestive tractnervous plexuses r severely injured& most neurons r destroyed.
y This results in disturbances of GIT
motility with frequent dilatationsin some areas.
y E fact that GIT receives abundantinnervations from e ANS system
provides an anatomic explanation
of e widely observed action ofemotional disturbances on GIT.
MUSCULARISPROPIA
y Contains smooth m/s arranged into inner circular & outer longitudinal layer.
y E contraction of this muscle causes peristalsis.
y Contains Myenteric or Auerbachs plexus that regulates e peristalsis.
ADVENTITIA/SEROSA
y E outermost layer of loose supporting type of connective t/s containing bloodvessels & nerves.
y Large amount of adipose t/s seen in fat individual.
y If e gut lies inside e peritoneal cavity will be lined by serosa (mesothelial liningepithelium).
-
8/9/2019 'Aliah's GIT & HB Systems1
3/33
THE HISTOLOGY OF TONGUE & ESOPHAGUS
PORTION DETAILS
TONGUE
STRUCTURE
y A muscular organ covered with mucosa.
y Its muscles are transverse, longitudinal, & oblique in arrangement which responsible for phonation, chewing, & swallowing.
y Properties:1. Mucosa: epithelial lining, dorsum & ventral surface, consists of 2 glands of epithelium & lamina propia (dense & glands
present).2. Connective t/s: presents around e connective t/s.
3. Blood vessels & nerves: presents in e connective t/s.4. Glands: serous & mucus embedded in e m/s.
PAPILLAE
1. Filiform papillae:
y
numerous.
y Have short bristles.
y Its core is a layer of dense connective t/s.
y Its surface has projection & keratinized.
y It is white in color.2. Fungiform papillae:
y They r scattered b/w e filiform.
y They r small red globular.
y Its core is rich in vascular connective tissue which gives e appearance of red color.
y Its surface is thin & non-keratinized.3. Circumvallate papillae:
y E largest papillae in size, but least in number.
y They r encircled by a cleft.
y Its side wall contains taste buds.
y Serous glands (Ebners glands) open into its base & secretes serous fluid which acts as solvent for taste provokingsubstance.
TASTE BUDS
y Act as chemoreceptors for taste sensation & gestation.
y Found in e human epithelium of circumvallate papil la of tongue & also scattered in other parts of tongue, palate,pharynx, & epiglottis.
y Each taste bud specializes in 2 of4 tastes.
y Approximately 3000 taste buds present.
y Life span is 10 days where renewal takes place.
y It is a barrel-shaped organ inside e full thickness of epithelium which opens at surface via taste pore.
y Each taste buds contains 50 spindle shape cells which consist of 3 types:1. Gustatory: light & long microvilli.
2. Dark sustentacular: supporting & long microvilli.
3. Basal cell: precursor of 1 or both of e cells.
SPECIALSENSATION
1. Sour or acid: lateral edge.2. Salt: tip of tongue.3. Sweet: tip of tongue.
4. Bitter: posterior portion of e tongue.
ESOPHAGUS
LAYERS
1. Mucosa:
y Stratified squamous epithelium.
y Muscularis mucosa: longitudinal smooth m/s.2. Submucosa:
y Contains elastic fibers for distension of bolus.
y Also contains small seromucous glands which prominent in upper & lower 3rd
of esophagus.3. Muscularis externa:
a. Upper 1/3: striated muscle.b. Middle 1/3: both striated & smooth muscle.c. Lower 1/3: smooth muscle.
THE HISTOLOGY OF STOMACH
PORTION DETAILS
OVERVIEW
y Functions:1. Continues e digestion ofCHO initiated in e mouth.2. Adds acidic fluid to food.
3. Promotes e initial digestion of protein with pepsin.
y E layers:
1. Mucosa: Lined with simple columnar epithelial cel ls characterized by mucous cap which protects from acidic condition.
When empty, it is thrown into longitudinal folds called rugae together with e submucosa.
Its surface is invaginated into gastric pits into which e gastric glands empty their secretion.2. Lamina propia: consists of loose connective t/s surrounded by thin muscularis mucosa.
3. Submucosa: dense connective t/s.4. Muscularis externa:
Has 3 layers: inner oblique, middle circular, & outer longitudinal.
At e pylorus, e middle layer is greatly thickened to form pyloric sphincter.
-
8/9/2019 'Aliah's GIT & HB Systems1
4/33
CARDIACGLANDS
y R simple or branched tubular glands.
y Most cells produce mucus & lysozymes, but few parietal cell s which secrete HCl can be found.
BODY &FUNDUSGLANDS
1. Surface mucus cells:
y Luminal space & foveolae.
y Contain mucigen granules.
y Stained poorly with H&E stain.
y Have short surface microvilli.
y Secrete HCO3-directly into e deeper layer of surface mucus coat.
2. Neck mucus cells:
y
Present in cluster or as single b/w e parietal cells in e neck & base region.
y Irregular in shape.
y Secrete mucus different from e one secreted by surface mucus cells.
y Have PAS negative material.3. Peptic or chief cells:
y Simple cuboidal or low columnar cells.
y Prominent at e lower region of e gland.
y Have basophilic granular cytoplasm.
y Have basally located nucleus which i s condensed.
y Its zymogenic granules contain e inactive enzyme pepsinogen which is converted into pepsin when released.
y Have rough endoplasmic reticulum4. Parietal or oxyntic cells:
y Large & pyramidal cells with intensely acidophilic cytoplasm.
y Scattered b/w peptic cells but more numerous towards e neck.
y EM shows e presence of intercellular canaliculli .
y Secrete HCl & glycoprotein intrinsic factors.
y Have an extensive eosinophilic cytoplasm.
5. Stem cells:
y Found at e neck region but few in number.
y Have oval nuclei near its base.
y Have a high rate of mitosis: Migrate upward to replace pits & surface cells. Migrate downward to replace mucus, parietal, chief, & entero -endocrine cells.
6. Enteroendocrine (Argentaffian) cells:
y Found at e base of e gland.
y Stained by silver or chromium staining.
y Produce histamine, enteroglucagon, & somatostatin.
PYLORUSGLANDS
y Have deep gastric pits with long, branched, & tubular pylorus glands.
y Most glands secrete mucus & contain several enteroendocrine cells:1. G cells: secrete gastrin which stimulates e secretion of acid.
2. D cells: secrete somatostatin which inhibits e release of some hormones.
THE HISTOLOGY OF THE INTESTINEPORTION DETAILAS
SMALL INTESTINE
LAYERS
1. Lamina propia:
y Loose connective t/s with VAN & lymphatics.
y In ileum, there r Pyeres patches (groups of lymphatic nodules).2. Muscularis mucosa:
y Thin layer of smooth muscle.
y May extend to e villi.
y Functions for rhythmic movement for absorption.3. Submucosa:
y Dense connective t/s.
y Contains Burners glands that open into crypts of duodenum which function to:
a. Secrete mucus alkaline (pH 8.1 9.3).b. Protects e duodenal epithelial cells against gastric juice.
CELLS
1. Columnar absorptive cells:
y Enterocytes: tall columnar cells.
y Contain numerous microvilli (striated border) at their apical surface.
y Function in absorption, fluid transportation, & synthesis of digestive enzymes.
2. Goblet cells:
y Unicellular flask-shaped mucous gland.
y Scattered among absorptive cells.
y Less numerous in duodenum & increase in no as approach e ileum.
y Function in lubrication & protection of e epithelium.
3. Paneth cells:
y Present in groups at e base of crypts.
y Large cells with large zyogenic secretory granules.
y Secrete lysozyme which digests e bacterial cell wall.4. Enteroendocrine cells:
y Similar in structure as those in stomach.
-
8/9/2019 'Aliah's GIT & HB Systems1
5/33
y Secrete many enzymes: secretin, chlecystokinin, somatostatin, serotonin, & vasoactive intestinal polypeptide (VIP).5. M (microfold) cells:
y Specialized epithelial cells overlying e lymphoid nodules of e Pyeres patches.
y Contain numerous membrane invaginations forming pits.
y Endocytose Ags & transport them to e underlying lymphoid cells.
SPECIALIZATIONTO INCREASESURFACE AREA
1. E small intestine is extremely long: 4 to 6 m.
2. Plicae circularis:
y Kerckring valves.
y Most prominent in e jejunum.
y Mucosa & submucosa r thrown as semilunaris circular or spiral folds.
3. Villi:y Finger-like projection of e mucosa.
y 0.5 1.5 mm long.
y Contain blood vessels & lacteal.
y Shapes:a. Duodenum: leaf shaped, broad, & long.b. Jejunum: finger shaped, narrow, & long.c. Ileum: smaller & apart from each other.
4. Striated border:
y At e apical surface of e simple columnar cells.
y Ahomogenous layer.
y Seen as packed microvilli in EM.5. Crypts of Lieberkuhn:
y E pits b/w e bases of e villi.
y Lined with glandular epithelium.
y Secrete intestinal juice.
LARGE INTESTINE
GENERAL
y Layers:1. Mucous membrane: neither plicae circularis nor villi.
2. Mucosa: thick, long deep crypts, with many goblet & absorptive (columnar with shorter villi) cells but fewenteroendocrine cells.
3. Lamina propia: contains lymphoid cells & nodules.
4. Muscularis mucosa.5. Submucosa.6. Muscularis externa: outer longitudinal & inner circular with taenia coli.
7. Serosa: contains appendices epiploicae.
y Functions:1. Absorption of water & mineral.2. Converting e residual chime into semisolid feces.
3. Absorption of some vitamins.4. Produces mucus.
APPENDIX
y Blindly ended evagination.
y Has a small narrow lumen with debris.
y Has a thick wall with fewer & shorter crypts with no taenia coli.
y Has many lymphoid nodules which extend to muscularis mucosa & submucosa.
ANAL CANAL
y Upper portion:
Has vertical folds called anal column which consists of mucosa & submucosa. Lined with simple columnar epithelial cell s with many goblet cells.
y Lower portion: non-keratinized stratified squamous epithelium which is continuous with that of skin.
y Submucosa:
Contains mucus glands called anal glands. Contains e terminal ramification of e superior rectal artery & veins. E veins form e hemorrhoid plexus which when enlarged constitutes e internal hemorrhoid.
y Muscularis externa:1. Inner circular: internal sphincter.2. Outer longitudinal: smooth m/s.3. Third longitudinal striated m/s: external sphincter.
y Adventitia.
-
8/9/2019 'Aliah's GIT & HB Systems1
6/33
THE ORAL ANATOMY: THE ORAL CAVITY
PORTION DETAILS
THE MOUTH CAVITY PROPER
y Mouth: from lips to palato-glossus arch (anterior p illars of fauces).
y Floor of e mouth: e space occupied by e tongue.
y Roof of e mouth: e hard palate & soft palate.
y Lateral wall: cheeks & inner surface of teeth & gum.
y Vestibule of e mouth: slit-like spaces where lips & cheeks lying b/w teeth & gum.
y Angle of e mouth: lies just in front of e 1st
premolar tooth.y Mouth cavity: e space inside e teeth & gum.
y E red transitional zone b/w the outer skin & inner mucous membrane of e lips is found only in man where h air follicles and sweat glands rabsent in this zone.
y Sensory nerve supply to e mucous membrane of e mouth:1. Roof: greater palatine & nasopalatine nerves.
2. Floor: lingual nerve & chorda tympani.3. Cheek: buccal nerve.
THE VESTIBULE
FEATURES
y It is e space b/w e lips and cheeks & teeth and gum .
y E lateral wall built from e cheek: buccinators m/s, buccopharyngeal fascia, & e skin.
y E parotid duct opens on e mucous membranes of e cheeks opposite e 2nd
upper molar tooth.
y Around e opening of e parotid duct, tiny molar glands open their ducts.
y Buccal & labial glands (mucous glands) r scattered in e vestibule, especially around e lower lip.
y Sub-mandibular and sublingual salivary glands open their ducts in the cavity of the mouth (not in the vestibule).
NERVE
SUPPLY
y Nerve supply of e mucous membrane of lips & cheeks:
1. Infra-orbital branch of maxillary: red marginal zone of e upper lip.2. Buccal branch of e mandibular nerve.3. Mental branch of inferior alveolar (from mandibular): for red marginal zone of e lower lip.
y Nerve supply of the gum:1. Upper gum:
a. Superior alveolar nerve.b. Greater palatine nerve.c. Naso-palatine nerve.
THE PALATINE TONSILS
y I.e.: e collection of lymphoid t/s at e lateral wall of e oropharynx.
y E surface is pitted, called crypts.
y Blood supply: ECA facial artery tonsillar artery.
y Lymphatic drainage: upper deep cervical LN.
y Relations:
1. Anterior: PG arch.2. Posterior: PP arch.3. Superior: soft palate.
4. Inferior: posterior 1/3 of e tongue.5. Lateral: capillaries, loose areolar t/s, sup. constrictor m/s,
styloglossus m/s, & facial A.
6. Medial: oropharyngeal cavity.
THE PARALINGUAL SPACE1. Location: deep to mylohyoid muscle which makes e dividing line b/w these 2 distinct spaces.2. Boundaries:
a. Lateral tongue including hyoglossus, styloglossus, & genioglossus.
b. Hyoid bone.c. Oral mucosa.
3. Contents:
a. Deep portion of submandibular gland. e. submandibular ganglion.b. Submandibular duct. f. hypoglossal nerve.
c. Sublingual curuncle. g. sublingual gland & fold.
d. Lingual nerve.
THE PLANE OF THE MOUTH
1. Superficial to mylohyoid: submandibular gland.2. Superficial to hyoglossus:
a. Deep lobe of submandibular gland.
b. Lingual nerve (CN III).
c. Hypoglossal nerve (CN XII).d. Submandibular duct.e. Sublingual gland.
3. Deep to hyoglossus:a. Lingual artery.
b. Glossopharyngeal nerve.
c. Stylohyoid ligament.
THE FAUCES
y I.e.: e space b/w e cavity of e mouth & e pharynx.
y E boundaries:1. Superior: e soft palate.2. Inferior: e root of e tongue.3. Lateral: e pillars of e fauces (PP & PG arches).
y E isthmus of e fauces: I.e.: e short constricted space that establishes e connection b/w
e oral cavity proper & e oropharynx. E boundaries:
1. Anterior: PG fold.
2. Posterior: PP fold.
2. Lower gum:a. Inferior alveolar nerve.
b. Buccal nerve.c. Lingual nerve.
-
8/9/2019 'Aliah's GIT & HB Systems1
7/33
THE ORAL ANATOMY: THE TONGUE
PORTIONS DETAILS
PARTS
1. Posterior 1/3 pharyngeal part:
y Post-sulcal part which is from sulcus erminlis to epiglottis.
y Known also as e root of e tongue or e base of e tongue.
y E function is for deglutition.
y E mucous membrane is smooth & contains lymphoid follicles (lingual tonsil part ofWalddeyers ring).
y It faces backwards forming anterior wall of e oropharynx.
y If it is touched, leads to nausea.
y It contains mucous and serous glands.2. Anterior 2/3 oral part:
y Pre-sulcal part or e body of e tongue which extends from tip to sulcus terminalis.
y Function is for mastication.
y It is freely mobile & faces upwards against e hard palate.
y It fills most of e mouth cavity & is loosely attached to e floor of e mouth.
y It has stratified squamous keratinizing variety.
y Its dorsum contains no glands but contains papillae (filiform, fungiform, vallate) which cause its mucousmembrane to be rough.
y E papillae contain taste receptors in e taste buds.
SURFACES
1. Dorsum:
y Posterosuperiorly located, partly in oral cavity & partly in oropharynx.
y Characterized by a V-shaped groove which is called terminal sulcus.
y E mucous membrane of e posterior 1/3 is thick & freely movable with underlying lymphoid nodules which iscalled lingual tonsil collectively.
y Shallow midline groove of e tongue: Divides tongue into Rt. & Lt. side.
Site of fusion of embryonic distal tongue bud.2. Inferior surface:
y Covered with thin & transparent membrane through which one can see e underlying veins.
y Connected to e floor of mouth through frenulum which allows e anterior part of e tongue to move freely.
y Sublingual curuncle present on each side of frenulum base including e opening of e submandibular duct.
BLOOD SUPPLY
1. Arterial supply:a. Dorsal lingual artery: posterior part & palatine tonsil.
b. Deep lingual artery: anterior part.2. Venous drainage:
a. Dorsal lingual vein: accompanies lingual artery.b. Deep lingual vein.
3. Lymphatic drainage:a. Superior deep cervical LN: posterior 1/3.
b. Inferior deep cervical LN: medial part of anterior 2/3.c. Submandibular LN: lateral part of anterior 2/3.d. Submental LN: apex & frenulum.
NERVE SUPPLY
1. Motor: all muscles r supplied by CN XII or hypoglossal nerve except palatoglossus muscle which is supplied by
pharyngeal plexus.
2. Sensation:1. General (touch):
y Mucosa of anterior 2/3 supplied by lingual nerve, branch ofCN V3.
y Mucosa of posterior 1/3 supplied by lingual branch ofCN IX.2. Special (taste):
y Mucosa of anterior 2/3 supplied by chorda tympani except vallate papillae.
y Mucosa of posterior 1/3 supplied by lingual branch ofCN 9.
MUSCLE DESCRIPTION ORIGIN INSERTION INNERVATION ACTION
EXTRINSIC MUSCLES: ALTER E TONGUES POSITION
GENIO-GLOSSUSFan-shaped muscle,
constitutes bulk oftongue.
Superior genital
spine of mandible.
Dorsum of tongue &
body of hyoid.
Hypoglossus nerve
(CN XII)
Protrudes apex of
tongue throughmouth.
HYO-GLOSSUSThin, quadrilateral
muscle.
Body & greater
horn of hyoid bone.
Side & inferior
aspect of e tongue.
1. Depresses tongue.2. Helps shorten
tongue.
STYLO-GLOSSUSSmall, short,
triangular muscle,fibers interdigitate
with hyoglossus.
Styloid process &stylohyoid ligament.
Draws tongueupward & backward.
PALATO-
GLOSSUS
Narrow crescent-
shaped palatine
muscle, acts as eboundary b/w mouth
& pharynx.
Palatine
aponeurosis of softpalate.
Side of tongue,blending with
intrinsic transversemuscle.
Pharyngeal plexus.
1. Elevates posterior
tongue ordepresses soft
palate.2. Constricts isthmus
of fauces.
INTRINSIC MUSCLES: ALTER E TONGUES SHAPE
SUPERIOR
LONGITUDINAL
Thin layer deep tomucous membrane of
dorsum.
Submucous fibrouslayer & medialfibrous septum.
Margins of tongue& mucous
membrane.
Hypoglossal nerve(CN XII)
1.Curls tonguelongitudinally
upward.
Branch of external carotid artery.
-
8/9/2019 'Aliah's GIT & HB Systems1
8/33
2.Elevates apex &sides of tongue.
3.Shortens tongue.
INFERIOR
LONGITUDINALNarrow band close to
inferior surface.
Root of tongue &body ohf hyoid
bone.
Apex of tongue.
1. Curls tongue
longitudinallydownward.
2.Depresses apex.
3.Shortens tongue.
TRANSVERSE
MUSCLEDeep to superior
longitudinal muscle.Median fibrous
septum.
Fibrous tissue atlateral lingual
margins.
Narrows & elongatestongue.
VERTICAL
MUSCLEFibers intersect
transverse muscle.Submucous fibrous
layer of dorsum.Interior surface ofborders of tongue.
Flattens & broadenstongue.
APPLIED ANATOMY
1. Gag reflex:
y Parlysis of genio-glossus tongue falls posteriorly suffocation.
y In anasthaesia e muscles is totally relaxed, therefore inserting an airway is essential.2. Fracture of mandible may lead to injury to e CN XII which causes atrophy of one side of e tongue. Thus, tongue will deviate towards e
paralysed side during protrusion due to e action of e unaffected genioglossus of e other side.3. Sublingual absorption of drug: (nitro-glycerine vasodilator-) in angina. Drug will be absorbed by e deep lingual nerve in less than a minute.4. Lingual carcinoma:
y Common & metastasizes to submental & submandibular regions and along e inferior jugular vein.
y CA at e ant 2/3 of e tongue: communication across midline (ipsilat metastases).
y CA at e post 1/3 of e tongue: network (bilat metastases).
5. Macro-glossia: big tongue.6. Micro-glossia: small tongue.
7. Aglosia: absence of tongue.8. Ankylo-glossia (adhesion): tongue tie.
9. Exessive length of frenulum: can lead to suffocation.
10. Bifid tongue (as in snakes tongue): double tongues.11. Trifid tongue: triple tongue.12. Congenital ligual cyst or thyroglossal cyst:
y Remnant of thyroglossal duct.
y Lies just cranial to e hyoid bone (central in position) can lead to dysphagia.
THE PALATES
PORTIONS DETAILS
GENERAL
y Form e arched roof of e mouth & e floor of e nasal cavities.
y It separates e oral cavity from e nasal cavities & e nasopharynx.
y E superior surface is covered with respiratory mucosa & e inferior surface is covered with oral mucosa which is densely packe d with palatine
glands.
y E blood supply: greater, lesser, & ascending palatine arteries as well as pterygoid venous plexus.
y E nerve supply: e greater & naso-palatine nerves (hard palate), e lesser palatine nerve (soft palate), & e pharyngeal plexus of nerve (all m/sof e soft palate except TVP by CN V2).
THE HARD PALATE
y Vaulted (concave) which filled by tongue when it i s a rest.
y E ant 2/3 has a bony skeleton formed by e palatine process of e maxillae & e horizontal plates of e palatine bone.
y E incisive fossa: a depression in e midline of e bony palate posterior to e central teeth into which e incisive canals open for e passing ofnasopalatine nerve.
y E foramina:1. E greater palatine foramen: e greater palatine vessels & nerve.2. E lesser palatine foramen: e lesser palatine vessels & nerve.
THE SOFT PALATE
FEATURES
y E movable post. 1/3 of e palate with no bony skeleton.
y Has 2 parts:
1. E aponeurotic part: e palatine aponeurosis (thick anteriorly & thin posteriorly) which attaches to e posterior edge ofe hard palate.
2. E posterior muscular part.
y Extends posteroinferiorly as a curved free margin from which hangs a conical process e uvula.
y Actions during swallowing:1. Initially: tensed to allow e tongue to press against it to squeeze e bolus to e back of e mouth.
2. Later: elevated posteriorly & superiorly against e wall of pharynx to prevent bolus entering e nasal cavity.
MUSCLES
1. Tensor veli palatini: tenses soft palate & opens mouth of auditory tube during swallowing & yawning.
2. Levator veli palatine: elevates soft palate during swallowing & yawning.
3. Palatoglossus: elevates post part of tongue & draws soft palate onto tongue.4. Palatopharyngeus: tenses soft palate & pulls walls of pharynx superiorly, anteriorly, & medially during swallowing.
5. Musculus uvula: shortens uvula & pulls it superiorly.
-
8/9/2019 'Aliah's GIT & HB Systems1
9/33
-
8/9/2019 'Aliah's GIT & HB Systems1
10/33
-
8/9/2019 'Aliah's GIT & HB Systems1
11/33
-
8/9/2019 'Aliah's GIT & HB Systems1
12/33
THE PANCREAS
PROPERTIES DETAILS
OVERVIEW
y An elongated, accessory digestive gland which produces 2 types of secretion:1. Exocrine secretion: pancreatic juice from e acinus which drains into 2np part of duodenum through pancreatic ducts.
2. Endocrine secretion: insulin & glucagon from e islets of Langerhans which enters blood.
y Lies:1. Retroperitoneally.2. Transversely across e posterior abdominal wall.3. Posterior to e stomach b/w e duodenum on e right & e spleen on e Lt.
y Its length is about 15 cm.
PARTS OVERVIEW ANTERIOR RELATIONPOSTERIORRELATION
OTHERS
HEAD
y Lies at e level of L2.
y E expanded part e gland thatis embraced by e C-shaped
curve of duodenum.
y Firmly attaches to e medialaspect of descending &horizontal parts of duodenum.
1. Transverse mesocolon.
2.Transverse colon.
3.Coils of jejunum.
1. IVC, Rt. & Lt. renalveins.
2.Aorta & Rt. renal
artery.3.Bile duct.
y Extension of
uncinate process, liesb/w:
1. Posterior: aorta &IVC.
2.Anterior: SMA.
y Rt. side: sup. & inf.pancreaticoduodenal arteries lies b/w ehead of pancreas &
e duodenum.
NECK
y Short (1.5 2 cm).
y E anterior surface is coveredwith peritoneum & is adjacent
to e pylorus of e stomach.
Gastroduodenal artery.1. E splenic vein.2.E SMV.
BODY
y Slopes gently upward & to eLt., passing over e aorta & L2
vertebrae.
y Possesses:1.3 borders: superior, anterior,
& inferior.
2.3 surfaces: posterior, inferior,& anterior.
1. Transverse mesocolon is
attached to e anterior border,
therefore:a.Anterior surface is covered
by e peritoneum of lesser
sac.b.E inferior surface is covered
by e peritoneum of egreater sac.
2.E inferior surface is covered
by:a.Duodeno-jejunal flexure.
b.Loops of jejunum.c.Lt. colic flexure.
1. Aorta & origin of
SMA.2.Lt. crus of
diaphragm & psoas
major m/s.3.Hilum of Lt.
kidney, Lt. renalvein, & Lt
suprarenal gland.
4.Splenic vein & IMV(in front of Lt. renal
vein).
TAIL
y Lies within e leino-renalligament.
y Relatively mobile & touches ehilum of e spleen.
y Related to colic flexure.
Lt. kidney.E tip is usually blunted
& turned superiorly.
BORDERS
1. Upper border:
a. Crosses e aorta at e level of celiac t runk.
b. Splenic artery runs along e upper border.2. Lower border: crosses e aorta at e level ofSMA.3. Anterior border: related to e transverse mesocolon.
PANCREATICDUCTS
1. Main pancreatic duct:
y Also called main pancreatic duct ofWirsung.
y It extends from e tail to e head of pancreas.
y It joins e bile duct at e hepato-pancreatic duct to
form e ampulla of Vater.
y E ampulla is guided by a circular m/s: sphincter ofOddi.
2. Accessory pancreatic duct:
y Also called accessory duct ofSantorini.
y If present, it drains e lower part of e head & euncinate process.
It crosses e main duct & opens at e minor duodenal
papilla 2 cm above e major papilla.
BLOODSUPPLY
1. Arterial blood supply:a. Head: sup. & inf. pancreatico-duodenal arteries of gastroduodenal artery.b. Neck, body, & tail: splenic artery.
2. Venous drainage:a. Splenic vein. All drain into portal vein.b. Sup. & inf. pancreatico-duodenal vein.
3. Lymphatics:
a. Pancreaticosplanic LN. Efferent vessels of these nodes drain into SM LN hepatic LN celiac LN.
b. Pyloric LN
NERVESUPPLY
y Parasympathetic fibers r exocrine in their function.
y They r carried via e posterior vagal nerve & celiac plexus.
y Sympathetic fibers r vasomotor & r carried by spinal nerve T6 to T10.
CLINICALIMPORTANCE
1. Early 2ndaries cancer of pancreas spreads to e liver via e portal vein.2. Pain fibers accompany e sympathetic fibers. Thus, pancreatic pain may be radiated in e distribution of e dermatome T6
to T10.
-
8/9/2019 'Aliah's GIT & HB Systems1
13/33
T
E
EEN
PROPERTIES DETAILS
OVERVIE
y A s
, v
s
u
s
us
ss
!
v!
y
!
!
"
!
s
# su !
,!
!
ysu
u
!
" y #!
!
u !
$ !
#
!
s # !
u .
y A% &
v&
'
(
, usu)
0 0y
1u
2
1 0 's
3,
1u
0 1y
4
)
ss)
5
&
u6
7
s'
8
7
9s
3
)
1
7 &
@
& % 7
s@
's
6
A
B
,C
,D E
F
4
G
.
y Weight about 150 g.
y Located in e Lt.u H H er abdominal quadrant or hy H ochondrium, b/I
e fundus of e stomach & e diaphragm where i treceives e protection of e lower thoracic cage.
y It forms e lateral extremity of e lesser sac.
SP RFAQ ES
1. Diaphragmatic surface:y Posterior surface which lies against e diaphragm & 9
th, 10th, & 11th ribs.
y Ribsseparate it from e Lt. pleura &lung.2.
R
isceral surface:
y Anterior surface which locates e splenic hilum.
y Its relations:a. Anteriorly:stomach. Splenic hilum lies b/w stomach & kidney.
b. Medially:Lt. kidney.
c. Inferiorly:Lt. colic flexure (on extreme lateral end of e spleen).d. Pancreas: b/w colic area & lateral part of splenic hilum.
BORDERS&ES DS
y 2 borders:
1. Superior border: Sharp & has one or two notches near its lateral end.
Lies b/w gastric area & diaphragmatic area.2. Inferior boder:
Rounded.
Lies b/w e renal area & e diaphragmatic area.
y 2 ends:1. Lateral end: anterior end (> expanded) & it reaches e midaxillary line.
2. Medial end: posterior end.
LIGAT EU TS
1. Gastro-splenic ligament:
y Peritoneal fold which isstretched b/w:a. V ilum of e spleen.b. Greater curvature of e stomach.
y Transmits:a. Short gastric vessels.
b. Lt. gastro-omental vessels.2. Leino-renal ligament:
y Peritoneal fold b/w:
a. Posterior abdominal wall.b. W ilum of e spleen.
y Transmits:a. Splenic vessel.
b. Tail of pancreas.
BLOOD &
NERVES
XPPLY
1. Blood supply:splenic vessels.
2. Lymphatics: pancreaticosplenic LN.3. Nerve supply:sympathetic via e celiac plexus (noradrenergic vasomotor).
CLINICALIMPORTANCE
1. E commonest abdominal organ to rupture by blunt trauma.2. Enlargement:
a. If e lateral border passes beyond e Lt. costal margin:doubled of e normal size.
b. When enlarged may reach e umbilicus.c. I hugely enlarged, e normal colic flexure resonance will disappear.
-
8/9/2019 'Aliah's GIT & HB Systems1
14/33
SMALL INTESTINE
PARTS EXPLANATION
DUODENUM- Sup. 2 cm part:
> Called ampulla
(duodenal cap).
> Immediatelydistal to pylorus.
> Has mesentery
> Mobile.
- Remaining part:
> Have no
mesentery
> Immobile because
retroperitoneal.
- C-shaped (around e head of pancreas), 1st, shortest (25 cm), widest, n most fixed part.
- Begins at e pylorus on e Rt. side n ends at duodenojejunal junc. (Level of L2, 2-3 cm to e Lt. of e midline n takes e formof acute angle called duodenojejunul flexure).
- Considered as partially retroperitoneal.
Superior (1st ) part. Descending (2nd ) part. Horizontal (3rd ) part. Ascending (4th) part.
- Short (5 cm), ascendsfrom pylorus.
- No circular folds andcontains submucosal
mucous glands.
- Proximal part:a) Sup.: Hepatoduodenal
lg.b) Inf.: Greater Omentum.- Peritoneum covers ant.
aspect, n bare post.
except e ampulla.
- Runs inferiorly, curvingaround HOD, 7.5-8 cm long,
n retroperitoneal- Initially, it lies to e Rt. of n
parallel to IVC.
- Bile n main pancreaticduct enter its posteromedial
wall n unite to form
hepatopancreatic ampullawhich enters major duodenal
papilla (posteromedially in
2nd
part)- Ant. surf. of proximal n
distal thirds covered withperitoneum.
- 10 cm long.
- Retroperitoneal- Runs transversely to e
Lt., passing over IVC,
aorta, n L3 vertebrae.- Crossed by SMA n
vein n root of
mesentery of jejunum nileum.
- Ant. surf. of horizontal
part is covered withperitoneum except e
crossing.
- Runs superiorly n along e Lt.
side of e aorta to reach e inf.border of BOP (2.5 cm).
- Here, it curves ant. to joinjejunum at duodenojejunal
junc., supported by e
attachment of suspensorymuscle of e duodenum
(ligament of Treitz).- e suspensory muscle passespost. to pancreas n splenic
vein n ant. to e Lt. renal vein n
attached to the right crus ofdiaphragm.
ANTERIOR Peritoneum, gallbladder,quadrate lobe of liver.
Transverse colon nmesocolon, coils ofSI.
SMA, SMV, coils ofSI.- Beginning of root of
mesentery, coils of jejunum.
POSTERIOR Bile duct, gastroduodenala., portal vein, IVC.
Hilum ofRt. kidney, renalvessels, ureter n psoas major
Rt. psoas major, IVC,aorta, Rt. ureter.
Lt. psoas major, Lt. margin ofaorta.
MEDIALHead of pancreas (HOP),
bile n pancreatic ducts. HOP.
VERTEBRAL LEVEL Anterolateral to L1 ontranspyloric plane.
Rt. of L2-L3 vertebrae. Ant. to L3 vertebrae. Lt. of L3 vertebrae.
SUPERIOR Neck of gallbladder.SM Vessels, HOP,
uncinate process ofpancreas.
Body of pancreas.
INFERIOR Neck of pancreas.
Jejunum Ileum
GENERAL
y Plicae circularis: series of transverse fold.
y Mucosa has small fingerlike projection(villi), which covered by simple columnarepithelium & carpeted by microvilli.
y Plicae n villi r tall & closely packed in proximal jejunum (mostabsorption), low & sparse in proximal ileum, & totally absent interminal ileum.
y Absorptive surface area is roughly 250 m2(size of a tennis
court).
OVERVIEW
- Begins at duodenojejunal flexure.- Most lies in e Lt. upper quadrant of e infracolic
compartment.- 2.5 m long.
- Ends at ileocecal junc. (3.5 m long).- Most of e ileum lies in e Rt. lower quadrant.
- Terminal ileum lies in e pelvis from which it ascends,ending in medial aspect of cecum.
COLOR Deeper red Paler pink
CALIBER 2-4 cm 2-3 cm
WALL Thick n heavy Thin n light
VASCULARITY Greater Less
VASA RECTA Long Short
ARCADES A few large loops Many short loops
FAT IN MESENTERY Less has windows More no windows
PLICAE CIRCULARES Large, tall, n closely packed Low n sparse, absent in distal part
PEYER PATCHES FewMany (present in mucous membrane found along ant-
mesenteric border)
MESENTERY
y Fan-shaped fold of peritoneum.
Average breadth of mesentery from its root tointestinal border is 20 cm
y Root of mesentery crosses ascending nhorizontal part of duodenum, abdominal aorta,
IVC, Rt. ureter, Rt. psoas major, n Rt. testicularvessels.
y Attaches jejunum n ileum to e post. abdominal wall .
y E root of mesentery (15 cm long) is directed obliquely,
inferiorly, n to e Rt., n extends from duodenojejunul junc. nRt. sacroiliac joint.
y Between 2 layers of mesentry are SM vessels, lymp h nodes,fat, n autonomic nerves.
MECKELSDIVERTICULUM
y This is a 0.44.8 inch (1.12 cm) long pouch that protrudes from the wall of the ileum.
y It is present at birth and represents the yolk stalk of the embryo. In most persons, the stalk structure disappears atbirth.
y It is not unusual, however, for Meckel's diverticulum to persist; it does not usually require treatment unless itbecomes inflamed or bleeds.
y 2 inches long, 2 feet away from ileocaecal junction, 2% of people-2/3 only true.
y Gastric or pancreatic mucosa is sometimes found in an ileal diverticulum.
y Complications: Diverticulitis, intestinal obstruction and intususception.
-
8/9/2019 'Aliah's GIT & HB Systems1
15/33
Lymphatic drainage of
duodenum
Blood supply of Small Intestine
Abdominal Aorta
Superior Mesenteric Artery
- Arises from abdominal aorta at L1,1cm
inf. to celiac trunk, runs between e layer of
mesentery.
- Sends 15-18 branches to e unum n ileum.
Arterial Arcades
- Loops of arteries
S lenic Vein
Superior Mesenteric Vein
- Drains jejunum n ileum.
- Lies ant. n to e right of SMA.
- Ends post. to e neck of pancreas
Vasa Recta
- Straight arteries
Portal Vein Vein
Blood supply of Small
Intestine
Lacteals intestinal Villi
L m hatic Plexus (wall of SI)
Lymphatic Vessels (layers of
mesentery)
Juxta-intestinal lymph nodes
(close to intestinal wall)
Superior central nodes (along
proximal pt. of SMA)
Mesenteric Lymph nodes
(among arterial arcades)
Sup. Mesenteric
Lymph nodes
Ileocolic Lymph Nodes
Perivascular nerve plexus (along SMA to e intestinal)
Symphatetic nerves (T8-T10) through symphatetic trunk nsplanchnic nerves (synapse in celiac n sup. mesenteric ganglia)
& Parasymphatetic nerves derives from posterior vagal trunk(synapse in myenteric n submucosa plexus)
Superior Mesenteric Plexusa) Symphatetic: reduces intestines motality n
secretion (vasoconstriction).b) Increases intestines motality n secretion, restoring
di estive abil it .
Blood supply of
duodenum
Abdominal Aorta
Celiac Trunk
Gasteroduodenal
Artery
Superior Mesentric
Artery/ Vein
- Part proximal to bile
duct into descending
part
- Part distal to e
entry of bile duct
Superior
Pancreaticoduodenal
Artery/ Vein
Inferior
Pancreaticoduodenal
Artery/ Vein
- Anastomose at e
level of entry ofbile duct
Portal
Vein
Splenic
Veins
Veins
Artery
Anterior
Lymphatic
Vessels
Posterior
Lymphatic
Vesels
Pancreatico-
duodenal
lymph nodes
Pyloric lymph nodes
> at gastero-
duodenal artery
Superior
Mesentric
Lymph Nodes
Celiac Lymph
nodes
At Superior n
Inferior pancreatico-
duodenal arteries
Vagus
nerves
Innervation of
duodenum
Greater n
Lesser
Splanchnic
nerves
Periarterial
Plexus
Celiac
Plexus
Superior
Mesentric
Plexus
-
8/9/2019 'Aliah's GIT & HB Systems1
16/33
-
8/9/2019 'Aliah's GIT & HB Systems1
17/33
-
8/9/2019 'Aliah's GIT & HB Systems1
18/33
Giardia lambia
POINTS DETAILS
OVERVIEW
y Disease: Giardiasis, lambiasis.
y Geographical distribution:1. Worldwide: > prevalent in developing world.2. > common in warm than in cool climate.
y Hosts:1. Man, especially children, less in adult.
2. Mice & rat can be infected.
MORPHOLOGY
TROPHOZOITE
y Size: 7 22 Y m, average: 14 15 Y m.
y Shape: bilaterally symmetrical, pear-shaped flagellate, broad & rounded anterior, taperingposterior end, & convex doral surface.
y
Sucking disk: ovoid, concave, occupies about of e flat ventral suface, bordered by ecurved intracytoplasmic portion of ant. flagella axoneme, & modified for attachment(mechanical irritation). Also used to resist ordinary peristalsis.
y Axonemes: straight, closely approximated, run parallel to each other dividing e body into 2halves through e whole length.
y Others: 2 nuclei with 2 large central karyosomes, 2 blepharoplasts, 2 deeply coma -shapedstaining bars considered to be parabasal bodies, & 4 pairs of flagella.
y Could be seen in diarrheic stool.
CYST
y Size: 10 14m.
y Shape: elipsoidal with a smooth, well-defined wall.
y Contains 2 or 4 nuclei, axostyle which r visible as 2 rods dividing cyst, parabasal bodies acrossaxostyle, & remnant of flagellae which r coiled.
y Under moist condition, cysts remain viable for months outside e host.
y More commonly seen in stool.
PHYSIOLOGY
1. Motion: e lashing flagella propel e trophozoite with a rapid, jerky, & twisting motion.
2. Nutrition: food is absorbed through intestinal content from epithelial cel ls through sucking disk.3. Reproduction:
y Multiplication occurs by mitotic division (longitudinal binary fission) during encystment, followed byseparation into daughter trophozoites after excystation.
y An alkaline environment, increased by achlohydria, & rich carbohydrate diet favor multiplication.
TRANSMISSION &INFECTION
y Through food & water contaminated with sewage, flies, or food handlers, & hand to mouth.
y Many outbreaks have been observed all over e world incl uding in day care centre & nurseries, most probably dueto contaminated water.
y It is > common in population practicing anal -oral intercourse.
PATHOLOGY
SITES1. Small intestine especially duodenum, jejunum, & upper ileum.2.Swim freely & rapidly in spiral motion & attached to intestinal epithelium.
3.Bile duct & gall bladder occasionally invaded.
PATHOGENESIS
y Only small no. of cyst r needed to initiate infection, as few as 10 cysts r able to produceinfection.
y Excystation occurs in e upper regions of e smal l intestine, where e parasites multiply by simplebinary fission.
y Prepatent period ranged from 6 15 days & usually lasted up to 41 days.
y Light infection r usually asymptomatic.
y Depends on: infection dose, genetic factors, achlorohydria, strain, acquired immunity, & local
secretory IgA deficiency.
MUCOSALFACTORS
y Mechanism of mucosal injury:1. Attachment of trophozoite to e epithelium can disrupt & distort microvilli.
2. Trophozoites produce cytopathic substances responsible for this disruption of epithelial
structure & function (proteinases & surface lectin).3. Produce proteinases which can find cleavage sites in proteins of e microvillus membrane.
4. Mucosal damage occurs by both mechanical & biochemical bindings & factors.
y Histologically:1. Mast cell mediated reactions contributes to e inflammation & edema seen in e mucosa &
lamina propia.
2. There is shortening of e villi & a cellular infilt ration of e lamina propia of e mucousmembrane.
y Disruption of intestinal structure:
1. Variable degrees of villous atrophy with associated crypt hyperplasia.2. Shortening & disruption of microvilli.3. Results in reduction in dissacharidase activities.
y Intestinal dysfunction:1. Impairment of intestinal solutes & electrolytes absorption.2. Impairment of glucose absorption.
COMPLICATIONS
1. Attachment to mucous membrane inflammation & hyperaemia diarrhea.
2. Associated with inability to absorb fats & vitamin A malabsorption fatty stool or steatorrhea.
3. Duodenitis duodenal irritation with excess mucous secretion) duodenal ulcer hunger pains picture of
peptic ulcer.4. Extra intestinal invasion cholecytitis.
5. Motility disturbance causes by parasites abdominal cramps.
CLINICALMANIFESTATION
1. Diarrheic syndrome in children & adults:
y Recurring or persistent diarrhea
y Irregular bowel movements.
y Epigastric discomfort & pain.
y Flatulence & loss of weight.3. Chronic symptoms:
2. Dyspeptic syndrome in adults stimulates gall bladder dyspepsia:
y Anorexia, nausea, & vomiting.
y Epigastric pain.
y Alternating diarrhea & constipation.
y Flatulence.4. Clinical complication:
-
8/9/2019 'Aliah's GIT & HB Systems1
19/33
a. Intermittent diarrhea.b. Impaired digestion.
c. Lactose intolerance.
d. Significant weight loss.
y Retardation of growth & development.
y Allergic & inflammatory conditions.
y Protein-loosing enteropathy.
DIAGNOSIS
1. Clinical picture.2. Copra antigen: disintegrated parasite identified by immunological
techniques asELISA.
3. Stool examination:
a. Macroscopically: Steatorrhea pale yellow & loose stool, lentil soupappearance, & contains excessive mucous & fat.
b. Microscopically: multiple cysts, no RBCs or Charcoat Leydencrystals, & presence of fat globules.In diarrheic stools, it isusual tofind only trophozoites.
4. Duodenal aspiration: if no cysts rpassed (contents may be
cultured).Duodenal content maybe sampled by e Enterotestcapsule which is gelatin capsule
containing a coiled thread.
5. Trophozoites may be detected by
endoscopic brush cytology or inmucosal impression smears os
small intestine biopsy.
TREATMENT
1. Metronidazol (flagyl):
y Should not be given to pregnant women.
y Adult: 250 mg, 3x/day.
y Children:5mg/kg body weight, 3x/day for 10days.
2. Tinidazol:
y Single dose of 2 g.
y Superior to metronidazol.
y Produces cure in 90%.
PREVENTION1. Treatment of cases.
2. Personal hygiene.3. Fly control
4. Proper water supplies & sewage disposal.
5. Chlorinating water does not kill e cyst, water should beboiled or filtered to remove e parasite.
LIFEa Ya LE b F c iardia lambia
Cysts are resistant forms and are responsible for transmission of giardiasis. Both cysts and trophozoites
can be found in the feces (diagnostic stages) . The cysts are hardy, can survive several months in cold
water. Infection occurs by the ingestion of cysts in contaminated water, food, or by the fecal-oral route
(hands or fomites) . In the small intestine, excystation releases trophozoites (each cyst produces two
trophozoites) . Trophozoites multiply by longitudinal binary fission remaining in the lumen of the proximal
small bowel where they can be free or attached to the mucosa by a ventral sucking disk . Encystation
occurs as the parasites transit toward the colon. The cyst is the stage found most commonly in non-diarrheal
feces . Because the cysts are infectious when passed in the stool or shortly afterward, person-to-person
transmission is possible. While animals are infected with Giardia, their importance as a reservoir is
unclear.
-
8/9/2019 'Aliah's GIT & HB Systems1
20/33
Ascaris lumbricoides
POINTS DETAILS
OVERVIEWy Probably earliest known worm.
y Also known as round worm (cacing gelang).
y Higher in cosmopolitan area.
y Normal symptoms r mild, but intestinal blockage can occur.
y Ectopic migration: pneumonit is ascariasis.
y Disease: ascariasis.
EPIDEMIOLOGY
y 1.3 billion r infected all over e world: 22% of
world population.
y 73% Asian population r exposed.
y 20,000 deaths per year in all over e world.
y Mode of infection: ingestion of infected eggsd/t contaminated food & water.
y Prevalence:
1. socio-economic.
2. Poor hygiene.
3. Poverty.
4. food intake.
y Modes of infection:1. Food & water contamination.2. Door knobs, furniture, paper
money, & fingers.
3. Air-borne (not much).
MORPHOLOGY
1. Adult worms:
y Size: male is 15 to 30 cm while female is 20 to 40 cm.
y 3 oval lips around mouth with sensory papillae to suck in food.
y Male worm has a coiled tail with spicule (used as sex identity).
y Female worm produces 20,000 eggs/day/worm.
y In 2 months, become higher in no in e ileum.
y Live span is 1 2 years.
2. Eggs:
y Measures 45 to 70 d m by 35 to 50 d m.
y Unsegmented when passed.
y In 2 weeks: e eggs contain e infective larvae.
y Withstand adverse conditions such as in Sahara oasis & etc.
y Susceptible to desiccation, dryness, r destroyed by direct sunlight within 15 hours, & r killed by temperature
above 40oC.
3. Larvae:
y Egg hatches in duodenum larvae penetrate intestine sojoumin in lung for 5 to 10 days migrate upthrough esophagus swallowed back.
CLINICALMANIFESTATION
Generallyasymptomatic or only
mild symptoms.
1. Larvae:
y Larva stage will cause:
a. Lung manifestations.b. Asthma-like: pneumonitis ascariasis & Loeffler syndrome
y Each larva in lung t/s 7 days.
y Continuous in endemic area & normally light infection.
y Sensitivity to repeated infection.
y Inflammation & hemorrhage in migration path: if the worm dies, granuloma formed.
y Signs & symptoms of pneumonitis ascariasis:a. Fever.b. Cough.c. Haemoptysis.
d. Dypnoea: contributory to Loeffler syndrome.
e. Eosinophils: Charcot Leyden crystal.
y sputum contain:
a. Charcot Leyden crystal.b. Eosinophils: modified.c. Ascaris: 4
thstage larvae.
y Seasonal: in S. Arabia, Vietnam, Laos.
y Prevalence: dry & wet season & t/out yr: countries w/o clear cut seasons.2. Adult worms:
y Severity of pathology depends on:a. Worm load:
1 worm: allergic response. < 10 worms: not so bad. both factors > 10 worms: severe. cause physical
b. Location of worms: blockage & few
< 1% gastric. worms r 12% ileum. asymptomatic. 87% jejunum.
y Intestinal irritation:a. Intermittent colicky pain & cramps.
b. Loss of appetite.
c. Fretfulness (resah).d. Protuberant abdomen (busong).
y Intestinal obstruction: It is commonest cause of acute intestinal obstruction in tropics where no. of worms r > 10. Mainly in children & rare in adults & prevalence is in lower socio-economic background. 2 types:
a. Acute: complete, small intestine, & mechanical.
b. Chronic: incomplete, large intestine, inflammation (tumour: stricture). Forms bolus-mechanical ileus in its common site, terminus ileum. Signs & symptoms: colicky pain, vomiting, constipation, dehydration, & distended abdomen.
Management: reassurance, rest, oral fluid (K+
replacement), antihelminth: albendazole (stat dose),
antispasmodic drug ( intestinal motility & maxolon - 0.2-0.4 mg/kg/dose), & surgery only if needed.
y Ectopic migration:
Presentations:a. Adults & children.
-
8/9/2019 'Aliah's GIT & HB Systems1
21/33
Life Cycle of Ascaris lumbricoides
b. Fever 102oF (esp. children)
c. Leads to anaesthesia.
d. Rx 4 yrs with antihelminthic & surgery (suture).
e. Worms emerge from:i. Mouth (mostly).
ii. nose (tracheal obstruction may be caused).
iii. eye (less common).
Migration of adult worm:
Male worms more often (smaller).
Enter any orifice & wounds.
Causes:
a. Block passage: appendicitis, ductus biliary blockage (may lead to calculi on death of worm &cholangitis), pancreatitis, & rarely enter hepatic vein (brain, heart, & lung).
b. Peritoneum: granuloma formation in organs.y Allergic manifestations:
Ag used isAscarissuum. Hypersensitive reaction.
Death of lab researches d/t allergy.
y Vilus atrophy (v.a): Caused byspiral movement.
Ratio of crypt:vilus.
Leads to nutritional impairment.
Malnourished children: protein loss & leads to kwashiorkor. Lactose intolerance. Absorption ofvitamin A, nitrogen & carbohydrate r affected.
Loss of plasma albumin.
Condition can be reversed by:i. Scheduled Rx (Rx11mnthRx2).ii. Supplement (food).
iii. Improve nutrionally.
COMPLICATION
1. Intestinal obstruction: commonest cause of death d/t intestinal blockage in children.2. Ectopic migration: high fever & anaesthesia.3. Adult worms migrate to unusual sites:
y Invasion of bile ducts, gallbladder, liver, & appendix.
y Migrate to peritoneal causing peritonitis.4. E byproducts of living or dead worms may rarely produce marked toxic manifestations in sensitized personssuch
as edema of e face,urticaria, insomnia, loss of apetite, & weight loss.
DIAGNOSIS1. Clinical manifestation: intestinal obstruction.2. Parasitological diagnosis: eggs in stool.3. Worm expulsion during treatment.
TREATMENT1. Albendazole:single 400 mg dose for 3 weeks repeated.2. Mebendazole: 100 mg twice daily for 3 days.
3. Control: avoid contamination of fodd & water.
Adult worms live in the lumen of the
small intestine. A female may produce
approximately 200,000 eggs per day, which
are passed with the feces . Unfertilized
eggs may be ingested but are not infective.
Fertile eggs embryonate and become
infective after 18 days to several weeks ,
depending on the environmental conditions
(optimum: moist, warm, shaded soil). After
infective eggs are swallowed , the larvae
hatch , invade the intestinal mucosa, and
are carried via the portal, then systemic
circulation to the lungs . The larvae
mature further in the lungs (10 to 14 days),
penetrate the alveolar walls, ascend the
bronchial tree to the throat, and are
swallowed . Upon reaching the small
intestine, they develop into adult worms .
Between 2 and 3 months are required from
ingestion of the infective eggs to oviposition
by the adult female. Adult worms can live 1
to 2 years.
-
8/9/2019 'Aliah's GIT & HB Systems1
22/33
HOOKWORM
POINTS DETAILS
EPIDEMIOLOGY
y Species:
1. Necator americanus: in Malaysia& South East Asia.2. Ancylostomaduodenale: in subtropic areas.3. Ancylostomaceylanicum: found inanimal but lower inhuman.
4. Ancylostomamalayanum: inMalaysia.
y Disease: anchylostomasis.
MORPHOLOGY
1. Adults:
y Size: female is 9 to 11 mm while male is 7 to 9 mm.y Male worms have spicule as copulatory organ.
y Live in 2nd
& 3rd
portion of jejunum & occasionally in duodenum.
y Have a large buccal capsule & cutting plate for damaging tissue to release blood.
y Also have one pair of anticoagulant gland to hold & suck in blood.2. Eggs:
y E no. of e eggs is fairly constant with 3000 to 6000 eggs/day/worm.
y 200 eggs at any one time.
y 4 to 8 cells when passed.
y Suitable condition for e eggs r warmth, shade, moisture, & sandy loam.3. Larvae:
y Infective larvae in 5 days.
y Amongst upper at about 2 cm of soil (3 6 weeks).
y Killed by direct sunlight.
y Larvae penetrate soft tissues (A. duodenale: penetration swallowed).
y Lung migration is short, only 24 hours.
y Mature in 2 months.
y Live span is 1 to 14 years.
PATHOLOGY
1. Larvae:
a. Skin penetration (from e soil):i. Human hookworm:
y Intense & ground itch (Local erythema, macules, & papules) in 7 to 10 days.
y D/t cutaneous invasion and subcutaneous migration of larva.
y Many larvae cause unrelieved pruritus which apparent as erythomatous popular rash.
y May lead to vascular rash by 2o
infection.
y Depends on e number of L 3.ii. Animal hookworm:
y Characterized by creeping eruption: cutaneous larva migrans.
y E migration is slow & gradual, not knowing e way to go.
y Caused by:
Anchylostomabraziliense. Anchylostomacaninum.
b. Lung migration- Loefflers syndrome:
y Pulmonary bronchitis, pneumonitis, & eosinophilia.
y Cough, dyspnea, & sore throat may present.y D/t migration of larvae through lung, bronchi, & trachea.
y Minute focal haemorrhage.
y Pharyngitis & laryngitis may occur in > number of L 3.2. Adults:
y Factors causing severity:a. Worm load, site of infection, & species.
b. Blood sucking activity for O2 & food.c. Changes in e location of blood consumption:
4 6 times a day.
Leads to ruptured capillaries which cause bleeding from mucosa.d. Status of host nutrition.
y Acute symptoms: < 2 weeks: fatigue, nausea, vomiting, burning & crumping abdominal pain , flatulence, & duodenitis.
2 6 weeks: diarrhea (red & black feces) & pallor (d/t anaemia).
y Chronic symptoms: Blood feeders which cause blood loss: light (3 mL) & heavy (100 mL).
Anaemia:
Iron deficiency anaemia (species dependent):a. Necator: normocromic normocytic (d/t smaller size & < blood consumption).
b. Ancylostoma: hypochromic microcytic - IDA (d/t larger size & > blood consumption).
Symptoms: pallor, edema (facia & pedal), cardiomegaly, Hb < 5 g/dL. Factors influenced:
i. Worm loads & species.ii. Iron reserves in host.iii. Iron daily intake.iv. Blood resorption.
v. Age of e host. Women r > affected than men.
Growth retardation.
Anorexia, epigastric pain & gastro-intestinal hemorrhage d/t attachment of adult worms & injury to upperintestinal mucosa.
Hypoalbuminaemia & edema d/t low haematological index.
-
8/9/2019 'Aliah's GIT & HB Systems1
23/33
Infantile hookworm dx: Occurred in China where infants r infected through contaminated diapers.
Symptoms: diarrhea, bloodystool,vomiting, anorexia, anaemia, & intestinal haemorrhage.
Now seen in Papua New Guinea.
Caused byA e f g ylostoma du h denale. Complication : 12% fatality with heart failure.
DIi
p N qr
Ir
y Diagnosis is made by identification of hookworm eggs in fresh orpreserved feces.
y Species of hookworms cannot be distinguished by egg morphology.
y Technique used:Harada Mori technique (increased detection & identification of species).
TREs
TMENT
y Mebendazole, 200 mg, for adults &100 mg for children, for 3 days is effective.
y Heavy infection:1. As above.2. Iron supplement.
3. Protein diet.
Et
IDEMIu LOGY&CONTROL
y Sanitation is e chief method of control:sanitary disposal of fecal material.
y Avoidance of contact with infected fecal material .
y Wearing shoes & personal health.
y Environmental: rainfall & plantations.
HOOKWORM LIFECYCLE
Eggs are passed in the stool (1), and under favorable conditions (moisture, warmth, shade), larvae
hatch in 1 to 2 days. The released rhabditiform larvae grow in the feces and/or the soil (2), and
after 5 to 10 days (and two molts) they become become filariform (third-stage) larvae that are
infective (3). These infective larvae can survive 3 to 4 weeks in favorable environmental
conditions. On contact with the human host, the larvae penetrate the skin and are carried through
the veins to the heart and then to the lungs. They penetrate into the pulmonary alveoli, ascend the
bronchial tree to the pharynx, and are swallowed (4). The larvae reach the small intestine, where
they reside and mature into adults. Adult worms live in the lumen of the small intestine, where
they attach to the intestinal wall with resultant blood loss by the host (5). Most adult worms are
eliminated in 1 to 2 years, but longevity records can reach several years. SomeA. duodenale larvae,
following penetration of the host skin, can become dormant (in the intestine or muscle). In addition,
infection byA. duodenale may probably also occur by the oral and transmammary route. N.
americanus, however, requires a transpulmonary migration phase.
-
8/9/2019 'Aliah's GIT & HB Systems1
24/33
Strongyloidesstercoralis
POINTS DETAILS
EPIDEMIOLOGY
y Also known as threadworm.
y Disease: Cochin-China diarrhea.
y Widely distributed: 3 to 30 mi llion cases (probably underdiagnosed).
y Female worms only r sufficient to maintain life cycle, this is known as parthenogenesis: e production of progeny w/ofemale & male copulation.
y Strongyloides fulleborni is commoninAfrica & Asia.
y Modes of infection: skin penetration & autoinfection.
MORPHOLOGYy E size of parasitic female is larger (2.2 mm x 45 micrometers) than the free -living worm (1 mm x 60 micrometers).y E male worm is 2 mm but is rarely seen.
y E eggs, when laid are 55 micrometers by 30 micrometers.
PATHOLOGY
y Light infections r generally asymptomatic.
y Severity depends on:1. Worm loads.2. Immunity of host.
3. Steroid treatment of patients.
y Larvae:1. Skin manifestation larva currens (running larva):
L3 penetration is rapid, but normally no ground itch.
Skin penetration causes itching & red blotches.
In sensitized persons.
L3 does not enter blood but migrates in skin causes diffused eruption for 2 3 cm broad. E speed is fast: rushes 10 cm/hr.
Lasts for 12 48 hours, but normally heals.
2. Loefflers syndrome:
L3 is capable of maturing to adult in lung & forms granuloma if dies. Causes bronchitis or asthmatic symptoms.3. During migration, e organisms cause bronchial verminous pneumonia & in e duodenum they cause a burning
mid-epigastric pain & tenderness accompanied by nausea & vomiting while diarrhea & constipation mayalternate.
y Adults: Asymptomatic in long duration.
Heavy infxn:
1. Intestinal irritation.2. Epigastric pain.
3. Vomiting.4. Loss of appetite.
5. body weight.
6. Eosinophilia 60-75%
Jejunum mucosa + submucosa:
1. eosinophils.
2. Villi flattened.3. Fibrosis of lamina propria.4.Malabsorption.
5. Enteritis. In immunocompromised patient:
Fulminating infection: dissemination of worm from jejunum to all organs. 50-70% fatal.
CF: diarrhea, hepatitis, myocarditis, pneumonitis, & CNS coma. Heavy, chronic infections result in anemia, weight loss & chronic bloody dysentery.
Secondary bacterial infection of damaged mucosa may produce serious complication s.
Cell mediated immunity may become defective or immunologically deficient. I f there is steroid therapy or organtransplantation, disease will disseminate & can lead to death d/t fulminating infection.
y In Papua New Guinea:
1985: over 100 cases causes epidemic. Affected 1 -3 years old child: swollen belly syndrome. CF: hyperinfection leads to pneumonitis & acute abdominal edem which r fatal.
DIAGNOSIS
y E presence of free rhabditiform larvae in e feces is diagnostic.
y Culture of stool for 24 hours will produce filariform larvae.
y S. fulleborni: eggs infeces.
y Through Harada Mori technique & culture.
TREATMENT
1. Creeping eruption: Thiabendazole.2. Intestinal:
a. Thiabendazole.b. Albendazole.
y S.s must be treated!
y Hyperinfxn unresponsive to Rx.
PREVENTION
1. Similar to hookworm.2. Prevalence underestimated.
3. immunocompromised patientt.
4. Shoes.
5. institutions mental hospital & prisons.
-
8/9/2019 'Aliah's GIT & HB Systems1
25/33
LIFE CYCLE OFv
trongyloiw x
sstercoralis.
The Strongyloides life cycle is complex among helminths with its alternation between free -living and
parasitic cycles, and its potential for autoinfection and multiplication within the host. Two types of cycles
exist: Free-living cycle: The rhabditiform larvae passed in t he stool (1) (see "Parasitic cycle" below) can
either molt twice and become infective filariform larvae (direct development) (6) or molt four times and
become free living adult males and females (2) that mate and produce eggs (3) from which rhabditiform
larvae hatch (4). The latter in turn can either develop (5) into a new generation of free -living adults (as
represented in (2)), or into infective filariform larvae (6). The filariform larvae penetrate the human host
skin to initiate the parasitic cycle (see below) (6). Parasitic cycle: Filariform larvae in contaminated soil
penetrate the human skin (6), and are transported to the lungs where they penetrate the alveolar spaces; they
are carried through the bronchial tree to the pharynx, are swallowed and then reach the small intestine (7).
In the small intestine they molt twice and become adult female worms (8). The females live threaded in the
epithelium of the small intestine and by parthenogenesis produce eggs (9), which yield rhabditiform larvae.
The rhabditiform larvae can either be passed in the stool (1) (see "Free -living cycle" above), or can cause
autoinfection (10). In autoinfection, the rhabditiform larvae become infective filariform larvae, which can
penetrate either the intestinal mucosa (internal autoinfection) or the skin of the perianal area (externalautoinfection); in either case, the filariform larvae may follow the previously described route, being carried
successively to the lungs, the bronchial tree, the pharynx, and the small intestine where they mature into
adults; or they may disseminate widely in the body. To date, occurrence of autoinfection in humans with
helminthic infections is recognized only in Strongyloides stercoralis and Capillaria philippinensis
infections. In the case of Strongyloides, autoinfection may explain the possibility of persistent infections
for many years in persons who have not been in an endemic area and of hyperinfections in immunodepressed
individuals
-
8/9/2019 'Aliah's GIT & HB Systems1
26/33
Enterobiy s vermicularis
POINT
DET
ILS
EPIDEMIOLOGY
y Also known as pinworm.
y Probably e commonest helminth infection.
y Difficult to diagnose.
y E worldwide infection is about 210 million.It is anurban disease of children in crowded environment
(schools, day care centers, etc.) with 1 12 years old is ehighest.
y Adults may get it from their children.
y Reinfection occurs in 30% of cases in 4 months.
y Reinfection original in 1 year.
y Disease: enterobiasis.
y Modes of infection:1. Autoinfection.2. Inhalation & dust.3. Toilet seats (family or institution infection).
4.C
lothessharing.5. Beds.
MORPHOLOGY
1. Adults:
y Female: 8 13 mm.
y Male: 2 15 mm.
y Female worms produce 10,000 to 15,000 eggs/worm/one time.2. Eggs:60 m x 27 m r ovoid but asymmetrically flat on one side.
PATHOLOGY
y Mainly asymptomatic.
y Can lead to loss of appetite & sleep.
y Pruritus ani:
D/t female worm migration. Deposition of eggs at perianal region.
Intense itching & scarification(d/t 2ndary infection).
Can lead to loss ofsleep or abnormal sleep position.
y Appendicitis: normally do not invade tissues.
y Migratory to lumen of cecum with no or rare
mucosal entry.
y Female worms go to e proximity of genitals:1. Pruritusvagiane.
2. Mucoid discharge.3. Urinary or genital disturbances.4. Gravid female worms go to fallopian tube:
salphingitis or endometritis.
y Eggs: rarely migrate (ectopic) to liver & lungsthrough blood & lymphatics.
CLINICALMANIFESTATION
y Attributed symptoms include:1. Anxiety.2. Irritability.3. Reduced emotional stability.
4. Nail biting.5. Nose picking.6. Teeth grinding.
DIAGNOSIS
y Diagnosis is made by finding e adult worm or eggs in e perianal area, particularly at night.
y Scotch tape or a pinworm paddle isused to obtain eggs: Done on waking up.
Before defecation & washing.
Dabbing: perianal area.
TREATMENTy Two doses (10 mg/kg; maximum of 1g each) ofPyrental Pamoate two weeks apartgive a very high cure rate.
y Mebendazole is an alternative.E whole familyshould be treated, to avoid reinfection.
y Bedding & underclothing must be sanitized between e two treatment doses.
PRE
ENTIONy Personal cleanliness (finger nails) providese most effective in prevention.
y Avoid sharing clothes like pajamas & bed.
y Take regular medication if problem persists.
LIFE CYCLE OF Enterobius vermicularis
Eggs are deposited on perianal folds (1). Self-infection
occurs by transferring infective eggs to the mouth with
hands that have scratched the perianal area (2). Person-
to-person transmission can also occur through handling of
contaminated clothes or bed linens. Enterobiasis may
also be acquired through surfaces in the environment that
are contaminated with pinworm eggs (e.g., curtains,
carpeting). Some small number of eggs may become
airborne and inhaled. These would be swallowed and
follow the same development as ingested eggs.
Following ingestion of infective eggs, the larvae hatch in
the small intestine (3) and the adults establish themselves
in the colon (4). The time interval from ingestion of
infective eggs to oviposition by the adult females is about
one month. The life span of the adults is about two
months. Gravid females migrate nocturnally outside the
anus and oviposit while crawling on the skin of the
perianal area (5). The larvae contained inside the eggs
develop (the eggs become infective) in 4 to 6 hours under
optimal conditions (1). Retroinfection, or the migration of
newly hatched larvae from the anal skin back into the
rectum, may occur but the frequency with which this
happens isunknown.
-
8/9/2019 'Aliah's GIT & HB Systems1
27/33
LOEFFLERS SYNDROME
PORTION DETAILS
Definition
y Infiltration of eosinophils lungs
y Dry cough
y Sputum with blood,CLC, larva (ascaris,strongyloides,HW)
y Dyspnae
y eosinophil count
y temporary in nature (seasonal in some countries)
y X-ray pneumonia suggestive
Etiologyy Ascaris lumbricoides
y Strongyloidesstercoralis
y Hookworm
Distributiony STH endemic area
y seldom recognized / reported
y children
Pathology &c/f
y Hypersensitive rxn to L3-L4 IgE mediated
y Symptoms may disappear after 7 days
y Lasting longer /seasonal / continuous ??
y Rx symptoms disappear confirms ascaris lumbricoides
Dx y Cf.TB, asthma,TPE:- Sputum larva,CLC
Rxy Supportive:
1. Antiallergic.
2. Antihelminth.
OTHERS REGARDINGINTESTINAL WORMS
PORTIONS DETAILS
PRE
ENTION &CONTROL
1. Improve sanitation.
2. Sewage disposal: night soil.3. Personal hygiene.
4. Supervision : children playground.5. Wearing shoes.6. Avoidance of indiscriminate defecation.
7. Health education.8. Biannual treatment.
STHINMALAYSIA
1. Polyparasitism:
y Rural areas.
y Squatter areas.2. Specific to low socio-economic groups.3. Overall infection rate: 43 94%.4. Prevalence:
a. Trichuris.b. Ascaris.
c. Hookworm.
5. Reinfection rates:
y High 32% in 4 months.
y E.v. in 6 months: 100%.6. Related to:
a. Hygiene.
b. Eating habits.
-
8/9/2019 'Aliah's GIT & HB Systems1
28/33
Trichuristrichiura
POINTS DETAILS
EPIDEMIOLOGY
y Also known as whipworm.
y Seen in cosmopolitan areas where e weather r warm & humid.
y Presently e commonest intestinal helminth.
y Disease: trichuriasis.
y Infection is through e ingestion of embryonated eggs via hands, food, or drink.
MORPHOLOGY
y E female organism is 50 mm long with a slender anterior (100 m diameter) & a thicker (500 m diameter)posterior end.
y E male is smaller & has a coiled posterior end.y E eggs r lemon or football (rugby) shaped & have terminal plugs at both ends.
PATHOLOGY
1. Pathology d/t:a. Adult worms attached to mucosal cells of caecum + upper colon
b. Severity depends on worm load.
c. Heavy worm burden: worms may reach rectum rectal prolapsed (30,000 eggs/gm of faeces).
d. Ulcers + 2o
infection (E. histolytica, B. coli, Shigella)2. Trichuriasis infection:
y Light infection: Normally asymptomatic.
Infection often seen with Ascaris. Normally is low worm burden.
Petechial + subepithelial haemorrhage Mucosal cell destruction
Mild diarrhea
y Heavy infection: Infection to rectum.
Bowel irritation d/t poor water resorption in colon .
Dysentery with blood & mucus: haematochezia & malaena. Abdominal pain, headache, & anorexia. Appendicitis: rare d/t Lumen blockage/irritation/inflammation.
Hypochromic anaemia:
800 worms average blood loss = 0.005ml/w/d.
Blood sucked / loss thru haemorrhage koilonychias.
3. Rectal prolapsed:
y D/t worms damaging e muscles.
y Straining to defecate.
y Normally in children.
y Swollen mucosa: reflex peristalsis.
4. Malnutrition:
y Very heavy infection.
y Growth retardation in children
y Stunting seen in sibling studies (cognitive ability also affected)
y Reversible (in some cases)5. Finger clubbing:
y Also known as kailonychia.y Nail is convex.
y 12% of heavy infection (in Malaysia).
CLINICAL FINDINGS
1. Abdominal pain.
2. Distension.3. Diarrhea/bloody.4. Headache.
5. Tenesmus.6. Anorexia.
DIAGNOSIS1. Clinical manifestation: rectal prolapsed with e worms seen.2. Diagnostic eggs in e stool.
3. Deformed eggs after treatment.
TREATMENT1. Albendazole: single 400 mg dose & repeat treatment is required.2. Mebendazole: 100 mg twice daily for 3 days.3. Rectal prolapsed: revert rectum & give t reatment for helminth.
PREVENTION
1. Treatment of infected individuals.
2. Sanitary disposal of human feces.
3. Washing hands before meals.4. Thorough washing & scalding of uncooked vegetable.5. Improve sanitation.
6. Sewage disposal: night soil.7. Supervision: childrens playground & Wearing shoes
8. Avoidance of indiscriminate defaecation.
9. Health education.10. Biannual Rx.
-
8/9/2019 'Aliah's GIT & HB Systems1
29/33
Life Cycle ofTrichuris trichiura
The unembryonated eggs are passed with the stool (1). In the soil,
the eggs develop into a 2-cell stage (2), an advanced cleavage stage (3),
and then they embryonate (4); eggs become infective in 15 to 30 days.
After ingestion (soil-contaminated hands or food), the eggs hatch in
the small intestine, and release larvae (5) that mature and establish
themselves as adults in the colon (6). The adult worms
(approximately 4 cm in length) live in the cecum and ascending colon.
The adult worms are fixed in that location, with the anterior portions
threaded into the mucosa. The females begin to oviposit 60 to 70days after infection. Female worms in the cecum shed between
3,000 and 20,000 eggs per day. The life span of the adults is about
1 year.
-
8/9/2019 'Aliah's GIT & HB Systems1
30/33
DRUGS IN PEPTIC ULCER DISEASE
PORTIONS DETAILS
OVERVIEWOF DISEASE
y A peptic ulcer is a break in e mucosa of e stomach (gastric ulcer) or duodenum (duodenal ulcer).
y Peptic ulcers r caused by an imbalance between e protective factors & damaging factors in e gastrointestinal mucosa.
y Factors that damage e mucosa: gastric acid, pepsin, H. pylori, bile acid, NSAIDS, smoking, & alcohol.
y Factors that protect e mucosa: mucus, bicarbonates, PG E 2, repair, & blood flow.
y Factors that influence e release of gastrin:
1. pH: pH, acid release.2. Food constituent.
3. Acetylcholine (ACh).y Factors that relates ACh with HCL secretion:
1. ACh binds with M-receptor at hystaminocytes histamine released proton pumps stimulated HCl secretion
increased.
2. ACh binds to M3-receptor at basolateral membrane of parietal cells proton pumps stimulated HCl secretion
increased.3. ACh stimulates gastrin secretion binds to gastrin receptor at histaminocytes proton pumps stimulated HCl
secretion increased.
4. ACh stimulates gastrin secretion binds to gastrin receptors at parietal cells (lower portion of stomach) proton
pumps stimulated HCl secretion increased.
DRUGS DETAILS
H2 RECEPTORANTAGONISTS
1. Overview:
y E.g.: Cimetidine, Ranitidine, Famotidine, & Nizatidine.
y First group or class of drugs for peptic ulcer.
y Mechanisms of action:a. Block histamine induced gastric secretion by binding to H 2 receptors.b. Decrease gastrin & Ach-induced gastric acid secretion.
c. Have antiulcerogenic effect: gastric ulcer d/t stress & drugs (NSAIDs, cholinergic, & histaminergic) is prevented.y They do not have any effect on gastric or esophageal motility or LES tone, thus reflux can occur.
2. Pharmacokinetics:
y Absorbed rapidly from e small intestine & not affected by presence of food in the stomach.
y Bioavailability is 60-80% due to first pass hepatic metabolism.
y Peak plasma concentration in 1-3 hours.
y About 2/3 of a dose is excreted unchanged in urine & bile, while e rest as oxidized metabolites.
y Dose reduction is needed in renal failure.
3. Adverse effects:
y Well tolerated by most patients, which occur in 5%. However, they r generally mild.
y Headache, dizziness, bowel upset, dry mouth, & rashes.
y Confusion, restlessness, hallucinations, delirium, convulsions & coma in some patients.4. Antiandrogenic effects:
y Possessed by cimetidine only (but not other H2 blockers).
y Displaces dihydrotestosterone from its cytoplasmic receptors which:a. Increases plasma prolactin.
b. Inhibits degradation of estradiol by liver.
y
High doses given for long periods have produced gynaecomastia, loss of l ibido, impotence & temporary decrease insperm count.
5. Interactions:
y Cimetidine inhibits cytochrome P-450 & reduces hepatic blood flow.
y It inhibits e metabolism of many drugs so they can accumulate to toxic levels, e.g. phenytoin, theophyllin,
phenobarbitone, sulfonylureas, metronidazole, warfarin, imipramine, nifedipine, quinidine, & etc.
y Antacids reduce absorption of all H2 blockers. When used concurrently a gap of 2 h. should be allowed.
y Ketoconazole absorption is decreased by H2 blockers.6. Uses:
a. Duodenal ulcerb. Gastric ulcer
c. Stress ulcers & gastritis
d. Zollinger-Ellison syndromee. Gastroesophageal reflux disease (GERD)f. Prophylaxis of aspiration pneumoniag. Other uses urticaria not responding to H 1 blockers.
7. Doses:
y On a scale of relative potency, ranitidine is more potent than cimetidine.
y
Famotidine is both more potent & has a longer half -life than either cimetidine or ranitidine.y Famotidine > Ranitidine > Cimetidine.
PROTON PUMPINHIBITORS
(PPI)
1. Overview:
y E.g.: Omeprazole, Lansoprazole, Pantoprazole, & Rabeprazole.y They inhibit e final step in gastric acid secretion & have overtaken H 2 blockers.
y They produce dose dependent suppression of gastric acid secretion; without anticholinergic or H 2 blocking action.
y They r powerful inhibitor of gastric acid: can totally prevent HCl secretion, without much effect on pepsin, intrinsic factor,juice volume, & gastric motility.
2. Mechanisms of action:
y Inactive at neutral pH PPI prodrug is converted to a Sulfenamide (active form) in acidic medium of parietal cell
canaliculi reacts with a cysteine residue on the H+K
+ATPase covalent disulfide bond formed inhibits e activity of
e proton pump irreversibly nearly complete suppression of acid secretion.
y For acid secretion to resume, e parietal cells must synthesize new H+K
+ATPase, which requires approximately 18 hours.
3. Pharmacokinetics:
-
8/9/2019 'Aliah's GIT & HB Systems1
31/33
y E oral absorption of omeprazole is 50% (u nstable at acidic pH), but as e gastric pH rises a higher fraction (up to ) maybe absorbed.
y It is highly plasma protein bound & rapidly metabolized by cytochrome P-450 in e liver & metabolites excreted in urine.
y Inhibition of HCl secretion occurs within 1 h, reaches max. at 2 h, is st ill half max. at 24 h & lasts for 3 days.4. Uses:
a. Peptic ulcer: omeprazole 20 mg OD. Relief of pain is rapid & excellent. Faster healing with 40 mg/day. Treatment
generally for 4-8 weeks.b. Required for anti-H.pylori therapy.
c. Drugs of choice for NSAIDs induced gastric or duodenal ulcers.d. Control bleeding from peptic ulcer (more effective than H2 blockers), i.v. pantoprazole preferred.
e. Gastroesophageal reflux disease (GERD).
f. Zollinger-Ellison syndrome. 60-120 mg/day or more of PPI is often required for healing of ulcers.5. Adverse effects:
y These r minimal: nausea, loose stools, headache, abdominal pain, muscle & joint pain, & dizziness (3-5%).
y Rashes (1.5%), leucopenia & hepatic dysfunction: infrequent.
y On prolonged treatment atrophic gastritis has been reported occasionally.6. Interactions: omeprazole inhibits e oxidation of certain drugs: diazepam, phenytoin, & warfarin levels may be increased.
PG E2ANALOGS
1. Overview:
y i.e.: misoprostol.
y PGE2 & PGI2 r produced in GI mucosa & appear to serve a protective role by inhibiting ac id secretion & promotingmucus & bicarbonate secretion.
y In addition, PGs inhibit gastrin production & increase mucosal blood flow.
y Natural PGs have a very short half-li fe. A no. of PG analogues with longer half-life have been developed.
y Ulcer healing in 4-8 weeks but poor reliever of ulcer pain.2. Adverse effects:
y Diarrhea, abdominal cramps, uterine bleeding, abortion & e need for multiple daily doses.
y Patient acceptability is poor.3. Uses:prevention of NSAIDs-induced peptic ulcer.
ANTICHOLINERGIC
AGENTS
y Pirenzepine: selective M1 cholinergic blocker.
y Gastric secretion is reduced w/o producing intolerable side effects.
y Usual doses inhibit acid secretion only by 40-50% (less than H2 blockers).
y Its therapeutic dose range is narrow: side effects occur with slight excess
ANTACIDS
1. Overview:
y Antacids r weak bases that react with gastric HCl to form water & salt.
y MOA: raise pH of gastric contents.
y Antacids do not decrease acid production.
y Acid-rebound occurs (-ve feed back mechanism) d/t increased gastrin release & gastric motility is increased.
y They are used on as -needed for symptomatic relief of dyspepsia.
2. Drug interactions: decrease the absorption of many drugs especially tetracyclines, iron salts, ketoconazole, H2 blockers,diazepam, phenothiazines, indomethacin, phenytoin, isoniazid, ethambutol, & fluoroquinolones.
3. Uses:
y Antacids r no longer used for healing peptic ulcer.
y They r now employed only for intercurrent pain relief, acidity , & minor episodes of heartburn.
ULCERPROTECTIVE
1. Sucralfate:
y Polymerizes at pH < 4 becomes a sticky gel like material strongly sticks to ulcer base remains there for 6 hr.y Precipitates surface proteins at ulcer base physical barrier preventing acid, pepsin & bile from coming in contact with
the ulcer base.
y It has no acid neutralizing action.
y Very little absorbed after oral administration.
y However, sucralfate is rarely used now because of need for 4 large well timed daily doses & the availability of simpler H 2blockers / PPIs.
y Dose: 1 g taken 1 hr before 3 major meals & at bed time for 4 -8 weeks.
2. Colloidal Bismuth Subcitrates (CBS):
y It is water soluble but precipitates at pH < 5.
y Heals 60% ulcers at 4 weeks & 80-90% at 8 weeks.
y Mechanism of action not clear, probabilities r:a. Increases secretion of mucus & bicarbonate through stimulation of mucosal PGE 2 production.
b. CBS & mucus form a glycoprotein -Bi complex which coats the ulcer & acts as a barrier to HCl.c. Detaches H. pylori from the surface of mucosa & directly kills this organism which is involved in causation of ulcer &
relapses.
y Side effects r diarrhea, headache & dizziness.
y Dose: 120 mg hr before 3 major meals & at b ed time for 4-8 weeks.
y Milk & antacids should not be taken concomitant