Labrador Keratopathy
Transcript of Labrador Keratopathy
532 AMERICAN JOURNAL OF OPHTHALMOLOGY MARCH, 1973
and the manuscript of the second volume was nearly complete at the time of his death.
The Chicago Ophthalmological Society established an annual Krill Memorial Lecture in recognition of his contribution to ophthalmology. His family and friends established a Krill Memorial Fund for ophthalmic research, to be administered by the Department of Ophthalmology at the University of Chicago. The proceeds from the fund are dedicated to the continuing education of physicians and scientists interested in retinal diseases and function.
Dr. Krill is survived by his wife, Suzanne, and daughter, Eileen ; his mother, two brothers, and a sister.
Frank W. Newell
CORRECTION
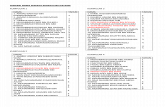
In the paper entitled, "The retinal surface in lattice degeneration of the cornea," by Barbara W. Streeten, M.D., and Melvyn Bert, M.D. (Am. J. Ophth. 74:1201, 1972),
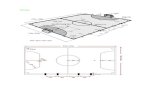
a part of Figure 1 was inadvertently deleted. This figure is correctly reprinted below.
CORRESPONDENCE
LABRADOR KERATOPATHY
Editor, American Journal of Ophthalmology:
Recently, D'Alena and Wood described a case of Labrador keratopathy with histologi-cal studies (Am. J. Ophth. 74:430, 1972). In their report, the material found in the cornea is described as hyaline and amorphous. They described vascularization at the periphery of the lesions in the cornea, a feature which has not been described in other reports of Labrador keratopathy. As in other reports of Labrador keratopathy, the authors described normal cornea between the sciera and the corneal lesions.
I recently completed a year-long study of 67 cases of band-shaped nodular dystrophy in the Bantu-speaking blacks of South Africa. I have graded the disease into five stages. Some cases falling into Stage 1 had no clear cornea adjacent to the sciera, the lesion extending up to the limbus. Stage 5 showed vascularization of the corneal lesions, as described by D'Alena and Wood, but in the cases in South Africa, this was invariably due to secondary infection. In the cases I saw, electron microscopy of the lesions showed essentially the same picture as shown by D'Alena and Wood—namely, a finely granular amorphous mass lying for the most part in the corneal epithelium and later in the stroma. Dr. Richard Green of the Wilmer Institute, Baltimore, examined sections of cornea with this dystrophy for me and found that the hyaline material gives a
Fig. 1 (Streeten and Bert). Lattice lesion after trypsin digestion. Peripheral retina is poorly vas-cularized, some arcades incomplete. Dark line across lower corner is artifactual fold. O = ora serrata (PAS-hematoxylin).
VOL. 75, NO. 3 CORRESPONDENCE 533
positive staining reaction for amyloid. The stain used was Congo red. I believe this to be the first report that the material found in the cornea in Labrador keratopathy is amyloid.
A full report of this study will appear in the second edition of the South African Archives of Ophthalmology.
Jeffrey Freedman, F.R.C.S. University of the Witwatersrand
Hospital Street Johannesburg, South Africa
EFFECTS OF AIR TRAVEL ON CONTACT-LENS WEARERS
Editor, American Journal of Ophthalmology:
Practicing near a large airport, I encountered a conspicuous frequency of corneal-ep-ithelial damage in contact-lens wearers who had just completed long, non-stop, high-altitude airplane flights. These cases included wearers well-adapted to their lenses with no recent ocular difficulties or changes in wearing schedule. After wearing their lenses during flight of several hours, slit lamp examination revealed a round or oval area of dense fluorescein staining from damaged or lost corneal epithelium in both eyes.
Disregarding cases in which other factors could have been operative (over-wearing of lenses, various evidence of other eye disease), there are still too many variables in the remaining cases to justify the formal publication of what I have encountered. In particular, I could not evaluate the adequacy of the fit of the lenses.
Transoceanic or non-stop transcontinental flights last at least four hours and such planes usually cruise at an altitude of 33,000 to 41,000 feet. The passenger cabin is pressurized and no oxygen or moisture is added to the air.
We know that a critical problem in the fitting of corneal contact lenses is interference by the lens with tear circulation and therefore with oxygen absorption by the cor
neal epithelium. A logical corollary is that during such a flight, despite adequate fit that allows tear circulation and oxygen transport, insufficient atmospheric oxygen and/or rapid tear evaporation may cause a "hypoxic cornea" syndrome. Could air travel precipitate this event?
Perhaps investigators able to control the variables and equipped to measure corneal oxygénation, tear evaporation, etc., under aircraft conditions could pursue the possibilities that my observations suggest. Also, lens fitters in high-altitude areas (e.g., Denver) might examine their experiences in terms of the local environment.
Louis S. Jagerman, M.D. 101 South San Mateo Drive
San Mateo, California 94401
NON-LYSOZYME ANTIBACTERIAL FACTOR IN TEARS
Editor, American Journal of Ophthalmology :
The article of Friedland, Anderson, and Forster (Non-lysozyme antibacterial factor in human tears. Am. J. Ophth. 74:52, 1972) raised several questions. The problem is as follows: The authors found that antibacterial activity of human tears, as measured by inhibition of growing Micrococcus lysodeic-ticus (lysoplate technique), was 200 times greater than would be expected from the actual amount of lysozyme present in tears as measured by a spectrophotometric assay. After heating of tears the activity on lysoplates was decreased and now correlated very well with the amount of lysozyme measured spec-trophotometrically.
I would kindly invite the authors to give additional information on the following points :
1. The spectrophotometric values (page 55)—These are expressed in mg H E L (hen's egg lysozyme)/ml of tears, by dividing units per ml (range from 24 to 100) by 20,000, the amount of units of lysozyme ac-